Case Quiz (April 2017)
A 12-year-old boy was presented with a history of gross hematuria and abdominal distention. The patient also had no history of previous surgical operation, blood transfusion, or use of hepatotoxic or nephrotoxic medications. The parents are not consanguineous, and there was no family history of liver or renal diseases. The physical examination revealed that his vital signs were normal; however, he had pallor, jaundice, hepatosplenomegaly, and ascites.
Laboratory investigations at presentation showed the following: hemoglobin 9 g/dl, platelets 133 × 10 9 /l, prolonged prothrombin time 16.9 s, prolonged partial throbmoblastin time 50.7 s, elevated total bilirubin 37 µmol/l (normal, <17 µmol/l), slightly elevated serum aspartate aminotransferase 51 IU/l (normal, 15–37 IU/l), normal alanine aminotransferase 29 IU/l (normal, 30–65 IU/l), normal alkaline phosphatase 172 IU/l (normal, 100–500 IU/l), normal γ- glutamyl transferase 86 IU/l (normal, 5–85 IU/l), low albumin 31 g/l (34–50 g/l), normal globulin 25 g/l (23–35 g/l), normal IgG level 11 g/l (normal, 5.4–16.1 g/l), normal IgA level 3.13 g/l (0.7–4.0 g/l), elevated IgM level 2.45 g/l (0.5–1.9 g/l), elevated blood urea 12.7 mmol/l (normal, 2.3–6.7 mmol/l), and slightly elevated serum creatinine 111 µmol/l (normal, 40–105 µmol/l). Serum C3 and C4 were 1.23 g/l (normal, 0.86–1.84 g/l) and 0.3 g/l (normal, 0.2–0.58 g/l), respectively. The urine examination showed proteinuria (3+), hematuria (red cell count 50 per field), red blood cell casts, and granular casts. The urine protein/creatinine ratio was elevated, 2.37 (normal, <0.03).
Further investigations with the use of upper gastrointestinal endoscopy showed gross esophageal varices, and ultrasonography of the abdomen revealed heterogeneous liver with irregular surface with splenomegaly and moderate ascites. Doppler ultrasound examination showed intrahepatic portovenous shunt and varices just posterior to the anterior abdominal wall. The chest X-ray and echocardiography were also normal.
Additional investigations revealed that serum α1-antitrypsin, copper, iron, and ceruloplasmin levels were normal. The urinary copper study was normal, as well as an eye examination. However, serum antismooth muscle antibody was positive at 1:40.
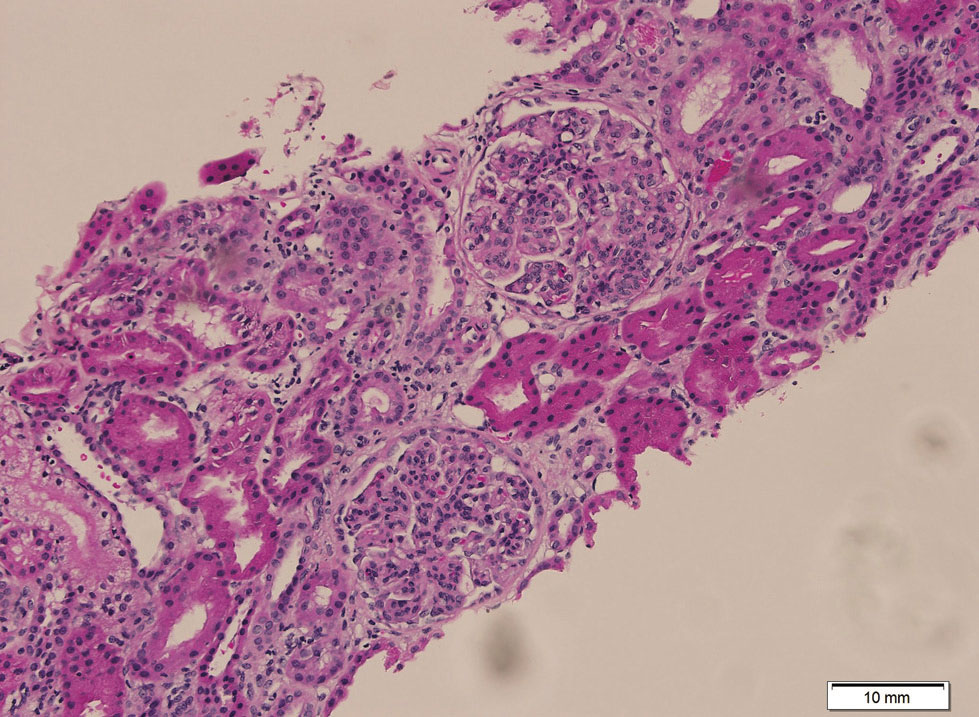
Renal biopsy was diagnostic
Case Answer (April 2017)
IgA nephropathy (IgAN) is commonly reported in adult patients in association with liver cirrhosis and portal hypertension. The pathogenesis of hepatic-associated IgAN is not fully understood. The abnormal clearance of the circulating immune complexes by hepatic Kupffer cells may allow them to access the systemic circulation with subsequent deposition in the kidney.
The differential diagnoses of concomitant liver and renal disease in children may also include the following: (1) conditions sharing the same etiology, such as congenital hepatic fibrosis and Caroli disease associated with autosomal recessive polycystic kidney disease, (2) chronic viral infection, such as chronic hepatitis B causing membranous nephropathy, or (3) renal impairment in a failing liver due to various causes, occurring as a terminal event, such as hepatorenal syndrome.