Case Quiz (December 2017)
A 12-year-old female child was admitted because of generalized weakness. She had no medical history and was not on any chronic medications. Her initial manifestations were fever, chills, weight loss (unintentional), palpitations, and night sweats for the past 2 months. Three weeks prior to admission, she developed a nonproductive cough. There was no past history of recent travel or sick contacts, den-tal/gastrointestinal procedure, poor dental state, colon disease, congenital heart disease, or hematological malignancy.
On physical examination, the child was pale and averagely nourished. Her temperature was 38°C, heart rate was 142 beats/min, blood pressure was 117/57 mm Hg, respiratory rate was 21 breaths/min, and oxygen saturation was 99% while breathing ambient air. Cardiovascular examination revealed tachycardia with a high-pitched holosystolic murmur at the apex, radiating to the back. There was basal crepitation. The patient did not present with any vasculitic features such as purpura, and neurological examination was unremarkable.
Blood tests showed normal kidney function with serum creatinine of 48 µmol/L and urea of 2.8 mmol/L. Her hemoglobin was 5.2 g/dL. The cause of anemia was attributed to acute inflammation (based on iron indices/reticulocyte count/negative Coombs test). Urine examination showed microscopic hematuria and proteinuria. Complement C3 was low and C4 was normal. Renal ultrasound showed normal-sized echogenic kidneys.
Transthoracic echocardiography was performed on admission which showed severe mitral valve regurgitation due to the failure of coaptation with a significant gap between the anterior and posterior mitral valve leaflet with vegetation. The left atrium and left ventricle were dilated. Left ventricular ejection fraction was 72%, and there was no evidence of pericardial effusion. The blood culture grew G. morbillorum which was sensitive to penicillin.
Her general condition continued to worsen in spite of antibiotics, and on the 3rd hospital day, she developed acute dyspnea with chest X-ray suggestive of pulmonary edema. Intra-alveolar hemorrhage was ruled out as the classical triad of hemoptysis, falling hematocrit, and diffuse infiltrates was absent. Diuretics were started. On the 7th hospital day, she developed acute kidney injury for which hemodialysis was required. The kidney ultrasound was unremarkable.
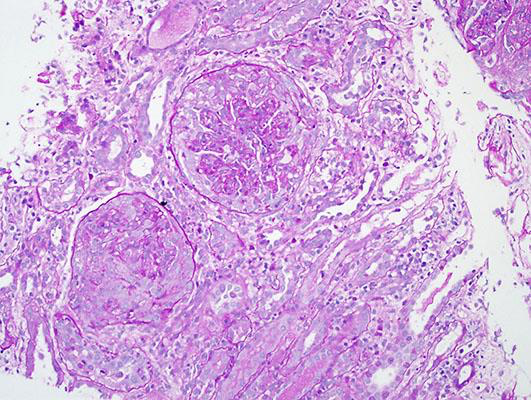
A renal biopsy was done on the 10th hospital day
Case Answer (December 2017)
Endocarditis-associated glomerulonephritis is mainly of immunological origin with deposition of immune complexes and C3 in the GBM.
Biopsy findings in cases of infective endocarditis with glomerulonephritis have been reported to vary from focal, segmental, or diffuse proliferative glomerulonephritis to crescentic glomerulonephritis. Among these, crescentic glomerulonephritis has been found to be the most common finding. Tubulointerstitial disease usually parallels the degree of glomerular injury. C3 staining has been invariably seen in almost all cases, with a smaller percentage of samples showing IgG staining as well.
Treatment of glomerulonephritis associated with endocarditis is controversial as some authors advise the use of immunosuppressive therapy combined with antibiotics, while others suggest the use of antibiotics alone.