Case Quiz (December 2022)
This patient started to suffer when he was one month old by picture of Chronic Kidney Disease (CKD). Kidney U/S revealed a picture suggestive of Autosomal Recessive Polycystic Kidney (ARPKD) and he was managed conservatively at that time. He developed GIT bleeding 4 years later which was explained by having Portal Hypertension and was controlled on propranolol. He passed to End Stage Renal Disease (ESRD) at age of 5 years, and he started regular Hemodialysis (HD).
He was prepared for kidney transplantation at age of 8 years. His father was the donor (39 years at time of transplantation without medical problems). Pre transplantation routine investigations were done (blood groups were A1 +ve {donor} & O+ve {recipient}, tissue typing revealed 2 out of 6 mismatches for B and DR alleles of HLA with negative donor recipient cross match by lymphocytotoxcity). Virology screen was negative for both donor and recipient for HCV, HBV, and HIV. Donor was CMV IgG positive while the recipient was CMV IgG negative for which prophylactic valgancyclovair was given. Right native nephrectomy was done intraoperativly. The operation was uneventful with smooth vascular anastomosis. Cold ischemia time was 70 min with adequate intra and postoperative fluid and electrolyte management.The child received non depleting antibody induction immunosuppression (basiliximab), maintainace triple therapy protocole (steroids, calcinurine inhibitors & mycophenolate mofetile) and infection prophylaxsis (Perioperative antibiotics, Sulphamethoxazol-Trimethoprim, Nystatin, Valgancyclovair).
He developed delayed graft function with high serum creatinine for 4 weeks post-operative during which HD was established. Graft ultrasound was normal but Doppler revealed increased resistivity index with picture was suggestive of Acute Tubular Necrosis (ATN). Graft biopsy was done day 14 post transplantation (Figure); the pathological findings supported the diagnosis of ATN with no evidence of rejection.
The child was re-biopsied 7 days later due to persistently impaired graft function. The later biopsy revealed persistent acute tubular injury, mild interstitial lymphoplasmacytic infiltarte involving about 30% of cortex (i2), scattered tubulitis with up to 4 lymphocyte/tubule (t1) with normal arterioles and peritubular capillaries (i.e., picture of persistent ATN with superimposed border line rejection). He received nondepleting monoclonal antibody (antithymocyte globulin) and pulse methyl prednisone therapy for treatment of rejection. ATN resolved 4 weeks postoperative and adequate graft function was established (serum creatinine declined to 1.1 mg/dL) and he was discharged on his triple immunosuppressive therapy and infection prophylaxis.
Six months post transplantation, the child presented with Urinary Tract Infection associated with impaired graft function. He was admitted and received empirical antibiotic and antifungal (Fluconazole) therapy till culture result available. Culture was negative and he developed transient attacks of gross hematuria. He had an attack of oliguria with rising serum creatinine when graft ultrasound revealed moderately sever backpressure changes and Doppler was unremarkable. Urine culture was repeated for bacterial and fungal growth and was negative for both.
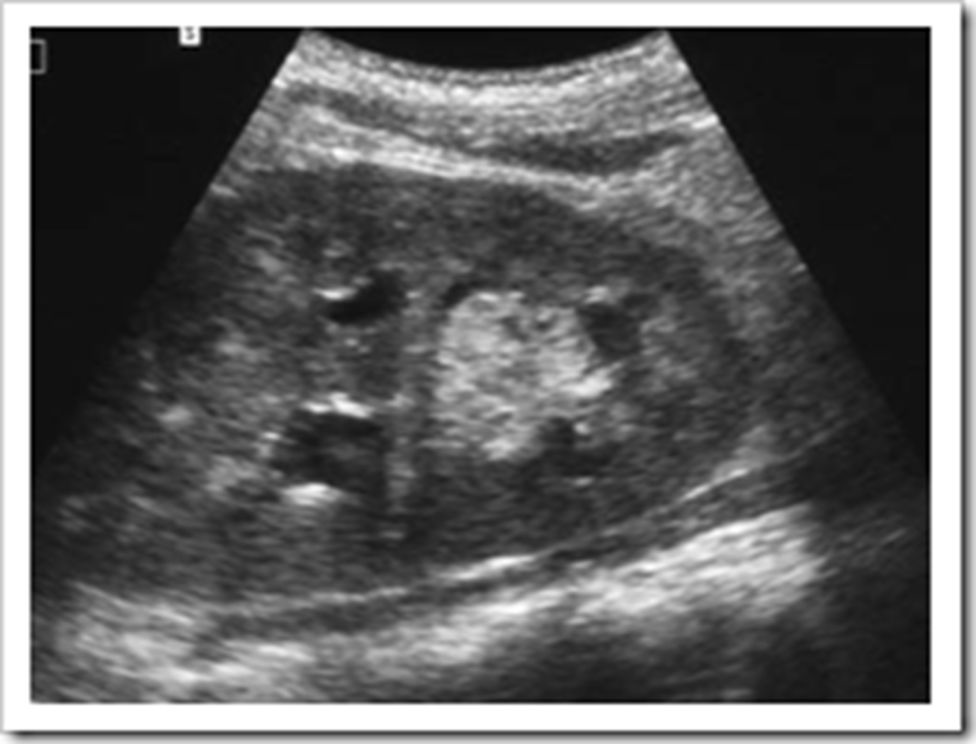
He developed an attack of anuria with rapidly rising creatinine up to 7.5 mg/dL. Urgent ultrasound revealed severe back pressure and increased echogenic contents with a distinct pelviureteric ill-defined small mass (Figure). HD started and urgent percutaneous nephrostomy was done to relieve the obstruction. Urine culture was repeated during this period and was still negative.
The diagnosis was established after analyzing nephrostomy tube urine. A successful treatment was able to slowly down the elevated serum creatinine and reverse the graft failure.

Case Answer (December 2022)
Localized Renal Graft Aspergillosis
Urinary tract aspergillosis occurs by three ways namely, ascending infection from the lower tract, from haematogenous dissemination or due to Aspergillus cast in renal pelvis. Immunosupression, UT instrumentation and prolonged antibiotic use are major risk factors
The child had negative urine cultures for fungal infection despite hematuria which could be explained by vascular invasion of the fungus that caused obstructed the pelvis later on by fungal mass. Renal aspergillosis is usually silent if the disease is localized to the cortex of the kidney. In this patient, fungal masse filled the pelvis of the graft causing hydronephrosis and later on obstructive anuria.
Diagnosis of this patient was provisionally made upon characteristic songraphic graft finding and was confirmed by fungal culture of the nephrostomy urine sample. Culture of the urine on Sabourad’s dextrose agar grew granular, brown–green colonies with a white apron suggestive of A. fumigatus.
