Case Quiz (March 2017)
A 5-year-old boy was admitted with the complaint of coughing and swelling of his whole body. He had a 10-day history of upper respiratory infection with mild coughing before admission.
His past history revealed no hematuria, proteinuria, rash, abdominal pain, or arthritis/arthralgia, and no family history of renal disease.
On physical examination there were periorbital edema and bilateral pitting edema of both legs. He was normotensive.
Laboratory studies revealed the following data: hemoglobin 11.7 g/dl, white blood cell count 10,900/mm3, platelets 192,000/ mm3, ESR 108 mm/h, total protein 3 g/ dl, albumine 1.49 g/dl, cholesterol 329 mg/dl, triglyceride 448 mg/ dl, and serum IgA 163 mg/dl. Serum electrolytes, AST, ALT, urea, and creatinine levels were within the normal ranges. Urinalysis revealed nephrotic range proteinuria (118 mg/m2/h) and microscopic hematuria. Complement C3 (138 mg/dl) and C4 (26 mg/dl) levels were normal and tests for antinuclear antibodies (ANA), HBsAg, and Anti HCV were negative.
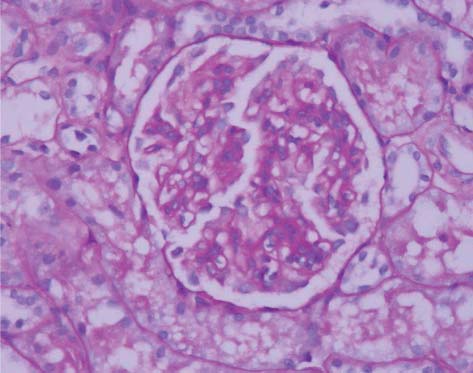
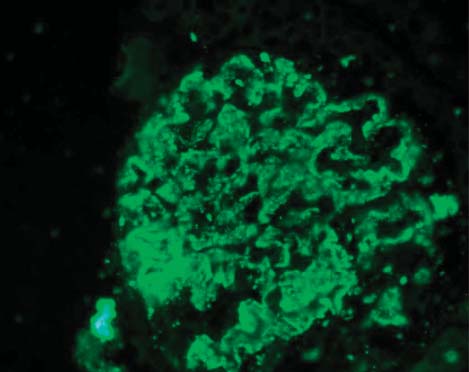
A percutaneous renal biopsy was performed because of the persistent proteinuria despite a full course of 4 weeks of steroid treatment (see figure)
Case Answer (March 2017)
IgA nephropathy is a form of glomerular disease usually diagnosed in patients with recurrent macroscopic hematuria or microscopic hematuria following a respiratory tract infection. Henoch-Schönlein purpura (HSP) and chronic liver disease should be considered in patients who show mesangial IgA deposition on kidney biopsy.
In this case, the renal biopsy showed an increase in the mesangial matrix, thickening of basement membrane, and different degrees of hypercellularity without tubulointerstitial changes. Immunofluorescence microscopy showed IgA, IgG, and fibrinogen deposition diffusely in the mesangium and basement membrane. The findings were consistent with IgAN.
Patients with IgA nephropathy develop proteinuria over time (sometimes early like the this case) and eventually they develop end-stage renal disease with risk of recurrence after transplantation.