Case Quiz (March 2018)
A 13- year-old girl was admitted with acute kidney injury. Three days earlier, she had had diarrhea, abdominal tenderness and fever. She has been taking thyroid hormone tablets for hypothyroidism. She was not on any other medications.
On admission, the patient’s height was 158 cm and her weight 51 kg. Her BP was 105/70 mmHg, HR 88 bpm, RR 24 breaths per minute and temperature 37.5C. Examination of the lungs and heart revealed no abnormalities, and there was no peripheral edema. Examination of the abdomen revealed diffuse abdominal tenderness, more severe in the umbilical area and in the right hypochondrium. The liver was palpable 3 cm below the right costal margin, and bowel sounds were diminished. The neurological examination revealed no abnormal findings. No skin rash or petechiae were observed.
Initial laboratory investigations revealed: Hb 12.4 g/dl, WBCs count 12.5 x10^9 /l (neutrophils 84%, lymphocytes 9%, eosinophils 1%), platelets 106 x 10^9 /l; one to two fragmented erythrocytes (schistocytes) per optical field were found on peripheral smear examination, and the reticulocyte count was 0.5%. Urea was 50 mg/dl and serum creatinine 5.6 mg/dl, while random glucose, serum sodium, potassium, total calcium, phosphorus and total bilirubin were normal; AST was 216 IU/l, and ALT was 229 IU/l, while GGT, ALP, total proteins and serum albumin were normal. Lactic dehydrogenase was 1,448 U/l and creatine kinase 975 U/l (normal, 50–240 U/l). Prothrombin time was 14.7 s (control 11–18 s), the INR 1.17, aPTT 138 s (normal, 25–38 s), fibrinogen 419 mg/ dl (normal, 150–350 mg/dl), fibrinogen degradation products 6 mg/ ml (normal, <5 mg/ml), D-dimers 0.5 mg/ml (normal, <0.5 mg/ml) and C-reactive protein 56.6 mg/l. The urine analysis revealed (++) proteinuria, 15–20 red cells (50% dysmorphic)/optical field. Chest radiograph and electrocardiogram were normal.
An ultrasound scan of the abdomen showed that both kidneys were of normal size (10.5 cm in length) without obstruction; the liver was moderately enlarged. The gallbladder appeared to contain granular precipitate (sludge), but there were no gallstones or dilatation of the biliary tree.
On day 1 after admission, the patient remained anuric; dialysis was initiated with fresh-frozen plasma. In the same night, the abdominal tenderness worsened, and bowel sounds were further diminished. An abdominal CT was performed. It showed a small amount of free serous liquid between bowel helices, a moderate diffuse hepatomegaly and a gallbladder with thick walls, giving an image of acalculous cholecystitis. Surgical intervention was deferred.
On day 2, the girl had fever (38C), was anuric with worsening thrombocytopenia (80 x 10^ 9 /l) and aPTT prolongation (>2 min). Immediately after termination of the second hemodialysis session (and after a weight loss of 0.5 kg), the patient presented signs of congestive heart failure. An M-mode cardiac echo showed global left ventricular hypokinesis with an ejection fraction of 50% (normal, 64–83%); a diagnosis of myocarditis, based on echocardiographic findings, was considered. ECG was normal. Troponin levels were 34 ng/ml (normal, 0–2 ng/ml). An empiric antibiotic treatment was initiated (metronidazole, ciprofloxacin).
The serologic investigation revealed: C3, C4 within normal limits, ANA (–), anti-DNA (–), anti-Sm antibody (–), anti-U1RNP (–), anti-Ro antibody (–), anti-La antibody (–), c-ANCA (–), pANCA (–), direct Coombs’ test (–) and haptoglobins 1.6 mg/l (normal, 0.5–2.0 mg/l). The microbiologic investigation revealed: negative stool cultures, negative blood cultures, negative urine culture, negative antibodies against hepatitis C, hepatitis B surface antibody (+), hepatitis A antigen (–), human immunodeficiency virus 1 (–), IgM antibodies against CMV, Epstein-Barr, herpes I and II virus, toxoplasma, Coxsackie’s B1-B6, rickettsiae and Hantavirus (–).
In color Doppler imaging of the renal vessels, there was no venous or arterial thrombosis, but the blood flow resistance index in both renal arteries at the renal hilum was elevated.
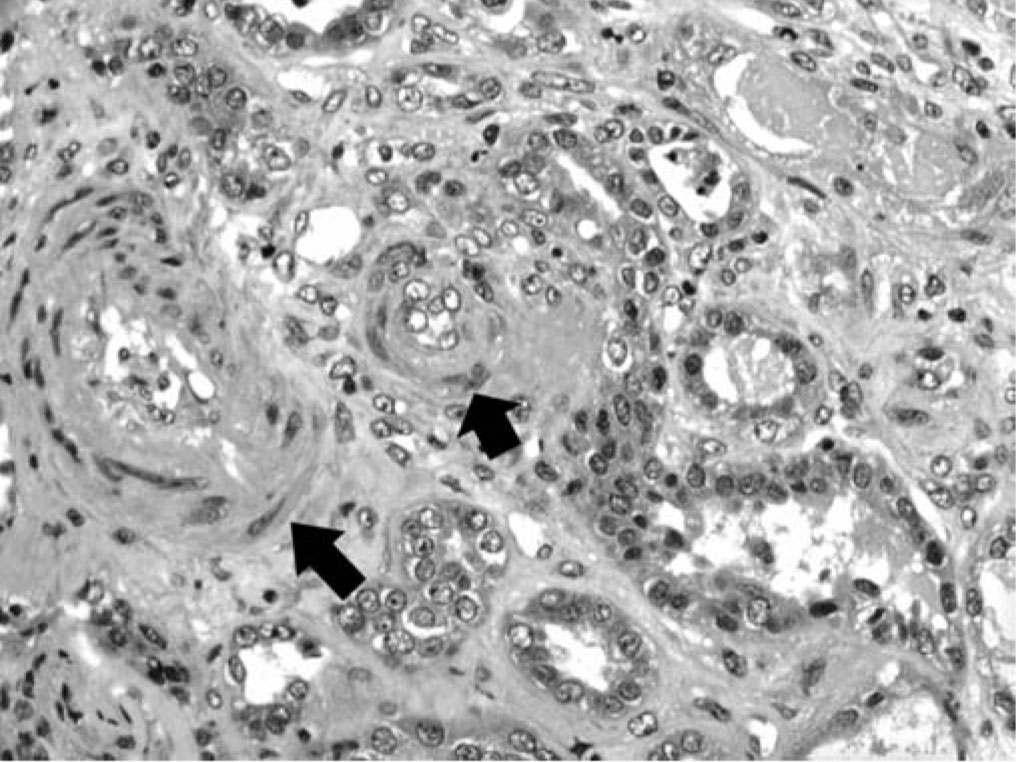
Renal biopsy was done (figure) and a diagnostic test was done
Case Answer (March 2018)
Catastrophic Anti-phospholipid Syndrome
The definite diagnosis requires four criteria to be fulfilled: (1) evidence of involvement of three or more organs and/or tissues, (2) development of manifestations simultaneously or within 1 week, (3) confirmation by histopathology of small vessel occlusion in at least one organ/tissue and (4) laboratory confirmation of the presence of an aPL (lupus anticoagulant and/or anticardiolipin and/or anti-b2 glycoprotein.
In the present case, renal, cardiac and hepatic-biliary involvement was present in the 1st week of the disease, acute TMA in the renal tissue was demonstrated, and the presence of aPL was repeatedly documented.