Case Quiz (October 2019)
A preterm boy presented with marked hyponatremia (plasma sodium of 104 meql/L) at the 21st day after birth. He was born at a gestational age of 31 weeks after an uncomplicated pregnancy, followed by spontaneous rupture of membranes and antenatal corticosteroid administration. Apgar scores were 8 and 9 at 1 and 5 minutes, and the birth weight was 2040 grams. There were no complications during NICU stay over the first 3 days of life.
An umbilical arterial catheter was inserted directly after birth, for the purpose of blood pressure monitoring, and removed after 4 days. Furthermore an umbilical venous catheter and subsequently a peripheral central venous catheter were inserted for the purpose of parenteral feeding. Routine cerebral ultrasonography showed an image consistent with the gestational age and mild periventricular flaring. No diuretics were administered.
At the fourth day of life the boy was transferred in good clinical condition to another hospital. He gained weight (from 1870 grams at the 4th day to 2090 grams at two weeks after birth). At the age of 3 weeks rejection to feeding (until this moment consisting of 150 mL/kg/day breast milk with breast milk fortifier), weight loss (to a minimum of 1960 grams), irritability, hyperthermia, and polyuria were noticed. CSF analysis showed 189 leukocytes/mm 3 with 11000 erythrocytes/mm 3 , after a traumatic lumbar puncture, thus a meningitis could no be excluded and intravenous antibiotics were started. Intravenous fluids, with a total volume of 150 mL/kg/day, containing 8 mg/kg/min glucose and 5 meq/kg/day sodium, were administered for 2 days (before return to the NICU).
The plasma sodium level had declined, from 140 meq/L nine days before, to 104 meq/L. The boy returned to the NICU under suspicion of a syndrome of inappropriate antidiuretic hormone secretion (SIADH) associated with the assumed meningitis, with initiated fluid restriction and sodium supplementation considered to be the appropriate therapy. The body weight at that time was 2040 grams.
On examination, he was pale, irritated with tachypnea, BP was 117/74mmHg, opisthotonus, and abnormal synchronized extensions of arms and legs. Laboratory analysis revealed a mild hypokalemia, hypochloremia, and hypomagnesemia, with normal calcium and phosphate levels. Plasma osmolarity was 219 mOsmol/kg, and urea and creatinine levels were normal. Blood gas analysis showed a respiratory alkalosis with normal bicarbonate. Infection parameters were negative, but liver enzymes and lactate were elevated (in the blood drawn several shortly after the seizure). Furthermore an elevated plasma B-type natriuretic peptide (BNP) of 1228 pmol/L was found. Urinalysis showed no leucocytes, mild hematuria, low sodium and potassium, with proteinuria, glucosuria, and a urine osmolarity of 129 mOsmol/kg. Cultures of blood, urine and cerebrospinal fluid revealed no microorganisms.
Case Answer (October 2019)
Hyponatremia, Hypertension Syndrome (HHS). The typical combination of symptoms in HHS was first described in 1952 in adults. In children, the syndrome is not encountered frequently and in neonates it is even more rare, with renal arterial stenosis following umbilical arterial catheterization.
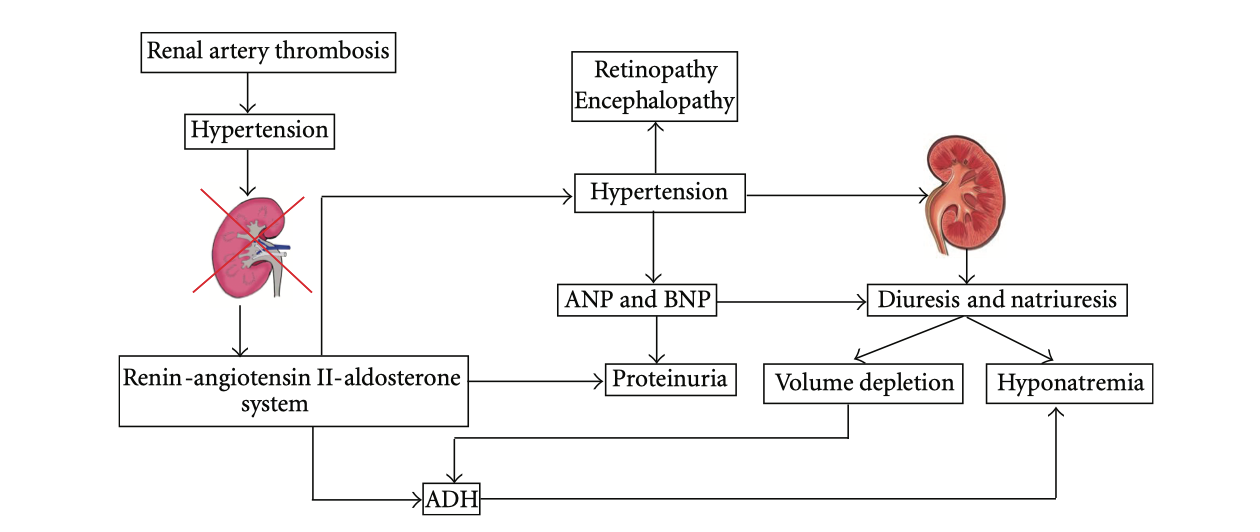
HHS is thought to be due to a complex interplay of different mechanisms, with unilateral renal hypoperfusion and a counteracting effect of the contralateral normal kidney as major hallmarks (“two-kidney-one-clip hypertension”).The renal arterial thrombosis causes hypoperfusion of one kidney, which activates the RAAS system to cause hypertension. The contralateral nonstenotic kidney reacts to this hypertension by excreting water and sodium (pressure diuresis and natriuresis). The hypertension additionally stimulates the cardiac atrial natriuretic peptide (ANP) and BNP to excrete more sodium and protein. The resulting hypovolemia, probably together with an increased production of angiotensin II, stimulates antidiuretic hormone (ADH), further aggravating the hyponatremia. Furthermore, aldosterone causes renal potassium loss, which in turn stimulates renin secretion, causing a vicious circle