Case Quiz (September 2016)
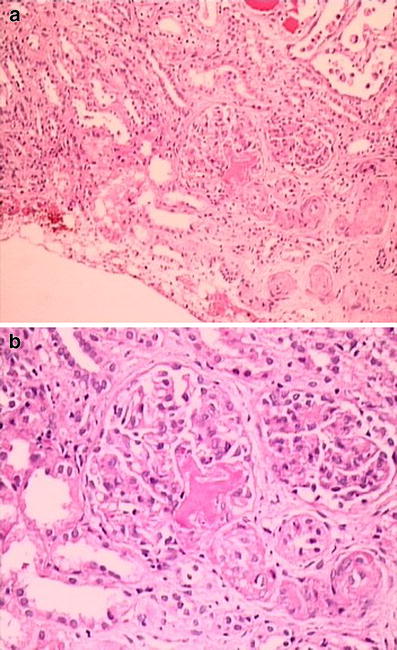
A 12-year-old girl was admitted due to abdominal pain, vomiting, loss of appetite, and diminished urine output for the previous 10 days. Consanguinity was present between her parents, and her maternal uncle had ESRD due to Alport syndrome. She seemed tired and weak and was dehydrated. Her weight and height were within normal ranges. Blood pressure was 250/170 mmHg, and heart rate was 120/min. A systolic murmur was heard on the left sternal border, and abdominal tenderness was detected on the right lower quadrant and around the umbilicus. Ophthalmologic examination revealed grade IV hypertensive retinopathy. Laboratory findings were as follows: hemoglobin (Hb) 10.5 g/dl, hematocrit (Htc) 30%, white blood cells (WBC) 14,200/mm3, platelets (Plt) 69,000/mm3, reticulocytes (Rtc) 16%, and the peripheral blood smear disclosed many fragmented erythrocytes. Blood urea was 33 mg/dl, creatinine 1.1 mg/dl, Na 129 mEq/L, K 2.6 mEq/L, total protein 6.9 g/dl, albumin 4.2 g/dl, AST 69 U/L, ALT 17 U/L, total bilirubin 2.8 mg/dl, conjugated bilirubin 0.66 mg/dl, and lactic dehydrogenase (LDH) 3,600 U/L. Urinalysis showed specific gravity 1.030, protein +++ (protein/creatinine ratio: 6.7 g/g creatinine), blood +++, and abundant red blood cells in the sediment. Na nitroprusside infusion was started for her severe hypertension. Direct Coombs, complement levels, coagulation tests, ANA, anti-dsDNA, ANCA, antiphospholipid antibodies, and factor H levels were normal. Renal ultrasound revealed a smaller right kidney (right kidney 75 × 34 × 30 mm; left kidney 114 × 50 × 46 mm), increased echogenicity in both kidneys , and a focal echogenic area on the upper part of the right kidney. Renal arterial and venous Doppler ultrasound was performed and was normal. Echocardiography showed concentric left ventricular hypertrophy and a left ventricular mass index (LVMI) of 87 g/m2.7 (upper limit of normal 38 g/m2.7). Haptoglobulin level was 0.5 g/dl (normal 0.3–2 g/dl). Renal biopsy was performed and revealed fragmented red blood cells and fibrin thrombi in the capillary lumina of the glomeruli (Figure). Glomerular basement membrane was thickened and showed wrinkling and double contour on periodic acid–Shiff (PAS) stain. Tubulointerstitium showed edema and mild inflammatory cell infiltration, and some tubules had red blood cells in their lumina. Electron microscopic examination also showed that glomerular basement membrane was thickened due to the swelling of lamina rara interna. What is the most likely diagnosis in this patient? What additional tests would you perform?
Case Answer (September 2016)
Malignant hypertension (MH) is a hypertensive emergency characterized by severe elevation of blood pressure and ischemic retinal lesions, including the presence of bilateral cotton-wool spots, flame shaped hemorrhages and papilledema. Thrombotic microangiopathy is a well-recognized complication of MH. It has been shown that endothelial dysfunction caused by activation of the renin–angiotensin–aldosterone system has a central role in the pathogenesis of MH.Patients with MAHA due to TTP/HUS typically have severe thrombocytopenia (<20,000/mm 3 ), hypertension but without retinal findings, history of TMA and/or thrombocytopenia without hypertension and no recovery of thrombocytopenia or hemolysis despite blood pressure control. On the other hand, extremely severe hypertension and past medical history of uncontrolled hypertension favor the diagnosis of MH. It is also important to know that the prognosis is more favorable—with good blood pressure control—than the other causes of TMA.